Folate vs Folic Acid: What Pregnant Women Need to Know

Is this safe to eat? 🥑
Scan any meal to instant pregnancy safety checks and nutrition insights.
Quick Answer
If there's one nutrient that deserves top billing during pregnancy—especially in those first crucial weeks—it's folate. Or is it folic acid? The terms get thrown around interchangeably, but they're not quite the same thing. And understanding the difference actually matters for how well your body uses this critical vitamin.
Folate (vitamin B9) plays an irreplaceable role in your baby's development, particularly in forming the neural tube—the structure that becomes the brain and spinal cord. Getting enough before and during early pregnancy can prevent up to 70% of neural tube defects like spina bifida.
This guide breaks down everything you need to know: folate vs folic acid, how much you actually need, the best sources, when to start supplementing, and what to do if you've just found out you're pregnant.
Folate vs Folic Acid: What's the Difference?
Let's clear up the confusion right away:
Folate
Folate is the naturally occurring form of vitamin B9 found in foods. It's present in leafy greens, legumes, citrus fruits, and other whole foods. Your body absorbs and converts dietary folate into its active form (5-MTHF or methylfolate) through a multi-step process.
Folic Acid
Folic acid is the synthetic, manufactured form of vitamin B9 used in supplements and fortified foods. It's more stable than natural folate (which degrades easily) and has a higher bioavailability—meaning more of it gets absorbed into your bloodstream.
Here's where it gets interesting: folic acid itself isn't biologically active. Your body must convert it into methylfolate before it can be used. This conversion happens in the liver and requires specific enzymes.
The MTHFR Factor
You may have heard about the MTHFR gene. This gene produces an enzyme that's essential for converting folic acid into its usable form. Somewhere between 10-15% of the population (and up to 25% in some ethnic groups) carry variants of this gene that reduce conversion efficiency.
For most people, this isn't a significant problem—folic acid still works. But for those with reduced MTHFR function, some research suggests that methylfolate (the pre-converted, active form) may be more effective. If you know you have an MTHFR variant, discuss supplement options with your healthcare provider.
✓ Bottom Line
For most women, standard folic acid supplements work perfectly well. The more important factor is getting enough, regardless of the form.
Why Folate Is So Critical During Pregnancy
Folate's claim to fame is its role in DNA synthesis and cell division. During pregnancy, cells are dividing at an extraordinary rate—especially in those first weeks when your baby's neural tube is forming.
Neural Tube Development
The neural tube forms between days 21 and 28 after conception—often before many women even know they're pregnant. This structure closes and develops into the brain and spinal cord. Inadequate folate during this window increases the risk of neural tube defects (NTDs):
⚠️ Neural Tube Defects
- Spina bifida: Incomplete closure of the spinal column, potentially causing paralysis, bladder/bowel dysfunction, and learning difficulties
- Anencephaly: Severe underdevelopment of the brain, which is fatal
- Encephalocele: Brain tissue protruding through a skull opening
A landmark Medical Research Council study found that folic acid supplementation reduced NTD recurrence by 72% in women who'd had a previous affected pregnancy.
Beyond the Neural Tube
Folate's benefits extend well beyond NTD prevention:
- Red blood cell formation: Prevents megaloblastic anaemia, where red blood cells are abnormally large and don't function properly
- Placental development: Supports healthy placental tissue formation
- Reduced miscarriage risk: Some studies associate adequate folate with lower early pregnancy loss
- Preterm birth prevention: Research suggests possible protective effects
- Heart development: May reduce risk of certain congenital heart defects
- Cleft lip/palate prevention: Some evidence for protective effect
How Much Folate Do You Need?
Recommendations differ slightly between organisations, but here's the general consensus:
📊 Daily Recommendations
| Stage | Daily Recommendation |
|---|---|
| Women who could become pregnant | 400 μg folic acid daily |
| During pregnancy | 400-600 μg folic acid daily |
| High-risk women* | 4,000-5,000 μg (4-5 mg) folic acid daily |
*High-risk includes: previous NTD-affected pregnancy, diabetes, obesity, epilepsy medications, or family history of NTDs. Source: NHS, ACOG, and CDC guidelines
The Timing Question
Here's the critical point many women miss: you need adequate folate BEFORE conception. The neural tube closes by day 28—often before a missed period confirms pregnancy. By the time you get a positive test at 4-5 weeks, the window for NTD prevention may have already passed.
This is why health authorities recommend that all women of childbearing age who could become pregnant take a daily folic acid supplement, regardless of whether they're actively trying to conceive.
If you've just discovered you're pregnant and haven't been taking folic acid, start immediately. While the optimal window may have passed, folate still supports ongoing development throughout pregnancy.
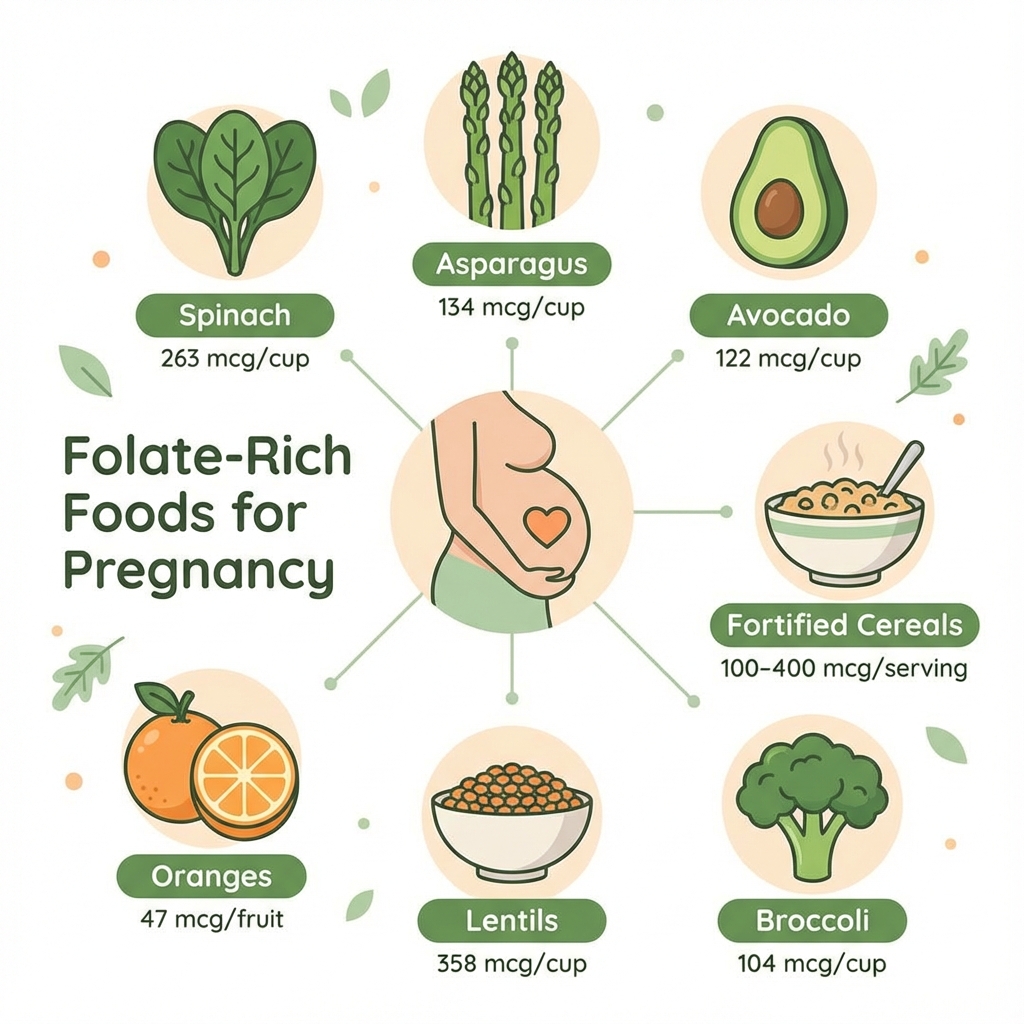
Best Food Sources of Folate
While supplements are essential (more on that below), food-based folate contributes to your overall intake and provides additional nutrients.
Top Folate-Rich Foods
| Food | Serving | Folate (μg) |
|---|---|---|
| Lentils (cooked) | 100g | ~181 μg |
| Spinach (cooked) | 100g | ~146 μg |
| Asparagus (cooked) | 100g | ~149 μg |
| Avocado | 1 medium | ~120 μg |
| Broccoli (cooked) | 100g | ~108 μg |
| Fortified breakfast cereal | 30g serving | 100-400 μg |
| Orange juice | 250ml | ~75 μg |
About liver: Beef liver is exceptionally high in folate, but comes with a caveat: it's also extremely high in vitamin A (retinol). Excessive retinol during pregnancy can cause birth defects. The NHS recommends pregnant women avoid liver and liver products entirely. Get your folate from other sources.
Cooking note: Folate is water-soluble and heat-sensitive. Boiling vegetables can destroy 50-90% of their folate content. Steam or stir-fry instead, and don't overcook.
Why Food Alone Isn't Enough
Here's the uncomfortable truth: even with an excellent diet, most women cannot reliably meet pregnancy folate requirements from food alone. Here's why:
- Natural folate has lower bioavailability (about 50%) compared to folic acid (85%+)
- Cooking destroys folate in many of the best sources
- You'd need to eat enormous quantities — roughly 500g+ of cooked spinach daily to hit 400 μg
- First-trimester nausea often makes eating vegetables difficult
- The critical window is before you know you're pregnant
This is why every major health authority—NHS, WHO, ACOG, CDC—recommends folic acid supplements for all women who could become pregnant. Food is important, but supplements provide the insurance policy.
Supplement Guidance: What to Take and When
Standard Recommendation
400 μg (micrograms) of folic acid daily, starting:
- Ideally, at least 1 month before conception (some recommend 3 months)
- Continue through at least the first 12 weeks of pregnancy
- Many prenatal vitamins provide 400-800 μg throughout pregnancy
High-Dose Supplementation (4-5 mg)
Your doctor may recommend this higher dose if you have:
- A previous pregnancy affected by NTD
- A partner with NTD or family history
- Diabetes (type 1 or type 2)
- Obesity (BMI ≥30)
- Coeliac disease or other malabsorption conditions
- Taking anti-epileptic medications (valproate, carbamazepine, phenytoin)
This higher dose requires a prescription—standard over-the-counter supplements don't provide this amount.
Methylfolate vs Folic Acid
Some supplements contain methylfolate (5-MTHF) instead of folic acid. This is the pre-activated form that bypasses the conversion step.
Who might benefit from methylfolate:
- Women with known MTHFR gene variants
- Those who've had issues with folic acid absorption
- Anyone advised by their healthcare provider
For most women: Standard folic acid is well-established, extensively researched, and effective. It's also typically cheaper. Unless you have a specific reason to choose methylfolate, regular folic acid works fine.
The Critical Timeline: When to Start
⏰ Timing Matters
| Before trying to conceive | Start 400 μg folic acid daily (ideally 1-3 months before) |
| Just found out you're pregnant | Start immediately if not already taking |
| Weeks 1-12 of pregnancy | Continue 400 μg folic acid daily |
| After week 12 | Continue through prenatal vitamin; standalone folic acid no longer essential |
The neural tube closes by day 28—that's only 4 weeks after your last period started, often before you know you're pregnant. If you're sexually active and could potentially become pregnant, consider taking folic acid as a precaution, even if you're not actively trying.
Special Considerations
If You've Missed the Early Window
If you discover you're pregnant at 6, 8, or 10 weeks and haven't taken folic acid, don't panic. Start immediately and continue through pregnancy. While the NTD-prevention window has passed, folate still supports:
- Ongoing cell division and growth
- Red blood cell production
- Placental health
- Your own energy levels
Most babies develop normally even without supplementation. The recommendation exists to reduce risk, not because deficiency guarantees problems.
Twins and Multiples
If you're carrying twins or more, some practitioners recommend higher folate intake due to increased demands. Discuss with your healthcare provider—you may need more than the standard 400 μg.
Medications That Affect Folate
Certain medications interfere with folate metabolism:
- Methotrexate (for autoimmune conditions)
- Anti-epileptic drugs (valproate, carbamazepine, phenytoin)
- Sulfasalazine (for inflammatory bowel disease)
- Metformin (for diabetes/PCOS)
If you take any of these, discuss folic acid needs with your doctor before pregnancy.
Knowledge Check
🧠 Scenario Quiz
Q: You've just found out you're pregnant at 5 weeks. You haven't been taking folic acid. What should you do?
A: Start taking 400 μg folic acid immediately. While the optimal window for neural tube closure (days 21-28) has likely passed, folate still provides benefits throughout pregnancy. Don't beat yourself up—just begin now and continue through at least week 12. Most babies develop healthily regardless of supplementation.
Common Questions
- Can I take too much folic acid? High doses (over 1,000 μg/day) for prolonged periods may mask vitamin B12 deficiency symptoms, which is problematic. Stick to recommended doses unless medically advised otherwise.
- Do I still need folic acid in the second and third trimesters? The critical period for NTD prevention is the first trimester. After week 12, folate remains beneficial but the standalone supplement is less essential. Most prenatal vitamins continue to provide adequate amounts throughout pregnancy.
- Is folate the same as vitamin B9? Yes—folate is vitamin B9. "Folate" refers to the natural form; "folic acid" is the synthetic form used in supplements and fortified foods.
- What if I can't swallow tablets? Folic acid is available in chewable tablets, gummies, liquid drops, and dissolvable tablets. Ask your pharmacist for alternatives.
- Does my prenatal have enough? Check the label—most contain 400-800 μg, which is adequate. You don't need an additional standalone supplement if your prenatal already provides enough.
The Bottom Line
Folate is genuinely one of the most important nutrients for early pregnancy. The evidence for its role in preventing neural tube defects is overwhelming and well-established. Here's what to remember:
- ✔ Start folic acid (400 μg daily) before trying to conceive — ideally 1-3 months before
- ✔ Continue through at least week 12 of pregnancy
- ✔ Food sources help but aren't sufficient — supplements are essential
- ✔ If you're just finding out you're pregnant, start now — it still provides benefits
- ✔ High-risk women may need prescription-strength doses — discuss with your doctor
- ✔ For most women, standard folic acid works fine — methylfolate is an option but not necessary for everyone
The neural tube closes before most women know they're pregnant. If you could become pregnant, treat folic acid like a non-negotiable daily habit—your future baby's brain and spine will thank you.
Related Reading
See also: Iron in Pregnancy, Calcium in Pregnancy, Protein Needs During Pregnancy, and Omega-3 During Pregnancy.
Download PregnancyPlate to track your folate intake and other essential pregnancy nutrients throughout your pregnancy journey.
Want to track your meals and check food safety instantly? Try PregnancyPlate — trusted by 50,000+ expecting mothers.



